Patient 2 weighs 20kg and is 0.7 metres tall. The drug dosage prescribed is 2mg/m2/day
As per the Mosteller formula, Body Surface Area (BSA) m2 (Mosteller, 1987)
= √ height (cm) x weight (kg) / 3600
Weight: 20kg; Height: 0.7 metres or 70 cms
√ 20kg x 70 cms / 3600 = √ 1400/ 3600 = √14/ 36 = 0.62 m2
If the dosage of drug is 2mg/m2/day, then the dosage will be
0.62 m2 x 2 mg = 1.24 mg /day
3e) Age of child = 6 years.
Recommended dosage 1 mg/years of age/day
1mg dose of drug for 1 year of child daily, then
For 6 years the dosage will be –
6 x 1mg = 6mg dose / day
3f) Age of child = 4 years
Recommended dosage 4.5 mgs/year of age/day
For 4 years the dosage will be –
x 4.5 mgs = 18/da
4.Volume of normal saline administered = 1.5 litres or 1500 mL
Time duration = 24 hours
The Drip Rate formula:
Drip Rate = Volume (mL) / Time (h) = 1500 / 24 = 62.5 ml / h (Park, 2013).
Therefore the patient will receive 62.5 ml of IV fluid every hour.
5. The given case scenario depicts that the patient, Emily is 88 years old. The patient is found to be in an independent state and her mental status is found to be alert. Respiration Rate (RR) of the patient was found to be 18 per minute scoring NEWS 2 score 0 (normal rate range 12 – 20 bpm); level of oxygen saturation is 80%, scoring NEWS 2 score 3 (normal level of saturation is ≥ 96); having blood pressure of 150/70, scoring NEWS 2 score 0 (normal systolic BP range 111 – 219); pulse rate of 92, scoring NEWS 2 score 1 (normal pulse rate range 51 – 90 bpm); and temperature of 37.5 ° C, scoring NEWS 2 score 0 (normal temperature range 36.1 – 38.0° C). The patient was found to be confused scoring 3 on NEWS 2 scale. Therefore aggregate NEWS 2 score of the patient Emily is 7 (Williams, 2019).
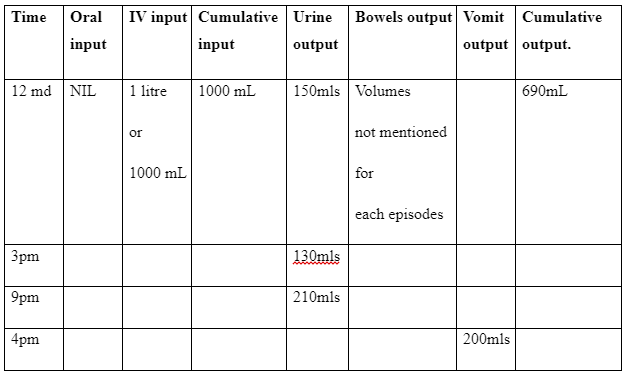
7. Normal output of urine should be 1ml/kg of body weight per hour. Here Christine has shown output of 490 ml of fluid within 9 hours. According to NICE, (2013) guidelines, the daily fluid or water administration can be up to 25 – 30ml/ kg /day. However, Christine was administered with 1000m
