As noted above, presence of antibodies because of past infection with one dengue serotype can predispose to more severe infection if exposure to a different serotype occurs. However, many infections are followed by long-lasting, sometimes lifelong, immunity. When infection with hepatitis A occurs in young children, infection is often mild or asymptomatic and often not diagnosed. With increasing age, severity of infection increases, and the case fatality rate may be 2% or higher in persons 65 years and older. Paradoxically, as availability of clean water and good sanitary facilities have improved in many countries, outbreaks of hepatitis A are now occurring, whereas they were unknown in the past when virtually everyone was infected and immune by age 5 years. By shifting upward the age at which individuals are infected, the virus causes acute, often severe clinical illness. Some countries that did not previously have visible hepatitis A outbreaks are now seeing large outbreaks in young adults.
Outbreaks Of Vaccine-Preventable Infections
Infections that have been prevented by immunization programs can re-emerge if immunization programs and other supports fail. After having been largely controlled for several decades, diphtheria re-emerged in the Russian Federation in 1990 and spread to all of the newly independent states and Baltic states of the former USSR (Dittmann et al., 2000) (Figure 3). Between 1990 and 1998, more than 157 000 cases and 5000 deaths were reported by countries of the former Soviet Union. Diphtheria, an acute bacterial infection caused by the toxin-producing bacterium Corynebacterium diphtheriae, which spreads from person to person through close contact, has a case fatality rate of 5–10%. Infection can be prevented by immunization with diphtheria toxoid; when infection occurs, mortality can be reduced by treating with diphtheria antitoxin. Universal childhood immunization was introduced in the 1940s and 1950s; developing countries also achieved high levels of immunization after the Expanded Program on Immunization (EPI) in the 1970s. Even before 1990, serologic studies had shown a substantial percentage of adults lacked immunity to diphtheria. Adults in the former Soviet Union who were in the 40–49-year-old age group in the 1990s had the lowest levels of immunity. They had lived during a time when diphtheria was largely controlled by immunization, so had not been exposed to natural infection. Most had never received any doses of vaccine since childhood, as adult booster doses were not recommended at that time. Toxigenic strains of diphtheria from Afghanistan were introduced into a refugee population. Infection spread first to large urban centers and then along major transportation routes to other cities and towns, and finally to rural areas. The spread was facilitated by the presence of large numbers of displaced persons. The proportion of cases in persons more than 15 years old was 64–82% in some areas. Relatively few cases occurred in adults aged 50 years or more, presumably because of past exposure to diphtheria, which was still occurring when they were children. The highest incidence and death rates were in individuals between the ages of 40 and 49 years. At the outset of the epidemic, the case fatality rate exceeded 20%, probably due to delayed treatment and lack of diphtheria antitoxin.
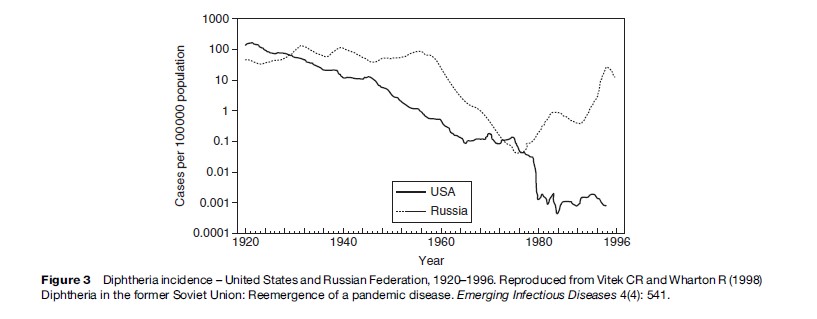
Multiple factors contributed to the massive outbreak as analyzed by Dittmann and colleagues (2000). Among those identified were: less intensive immunization, use of lower potency vaccine, antivaccine campaigns in some areas, deterioration of the health-care infrastructure, delay in outbreak control, and lack of adequate supplies for prevention and treatment in many areas. Other countries were also affected by the outbreak as cases were imported into several European countries and the United States. Most countries today do not routinely give diphtheria toxoid to adults; in many countries 30–60% of adults may be susceptible to diphtheria, which is a phenomenon created by the vaccine era and vaccine policy of giving vaccine primarily to young children.
