Patients present with several days to weeks of gradual onset of abdominal pain and tenderness, diarrhea and occasionally bloody stools (Figure 3(a)). This is different from bacterial causes of dysentery, where patients usually only have 1 to 2 days of symptoms. Surprisingly, fever is present in only the minority of patients with amebic colitis. Colonic lesions can vary from only mucosal thickening to flask-shaped ulcerations to necrosis of intestinal wall (Figures 3(b)–3(f )). Unusual manifestations of amebic colitis include toxic megacolon (0.5% of cases, usually requiring surgical intervention), ameboma (granulation tissue in colonic lumen mimicking colonic cancer in appearance), and a chronic nondysenteric form of infection that can present as years of waxing and waning diarrhea, abdominal pain, and weight loss (easily misdiagnosed as inflammatory bowel diseases).
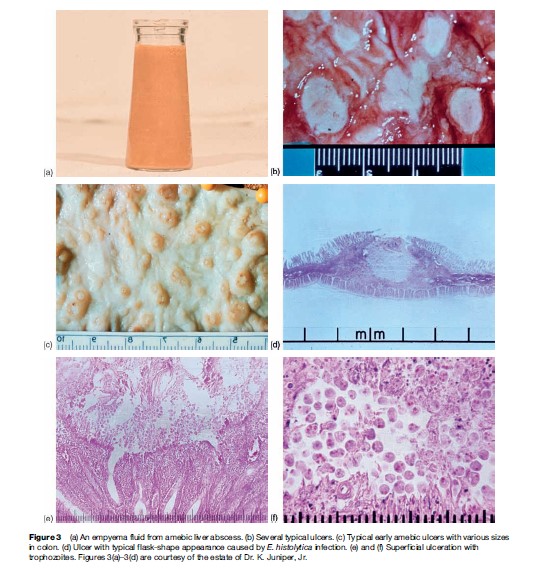
A heightened suspicion of amebiasis should be present if the patient has been in a developing country in the last year (as a resident or traveler). In a patient with diarrhea, if blood is present in the stool (grossly bloody or occult blood positive; Figure 3(a)), then infectious (Shiga toxin-producing E. coli, Salmonella, Shigella, Campylobacter, and E. histolytica) and noninfectious (inflammatory bowel disease, diverticulosis, arteriovenous malformations, cancer) causes should be considered. The diagnosis of amebic colitis is best made by antigen detection in stool (not widely available), by colonoscopy and biopsy, and by detection of antiamebic antibodies in serum (present in most but not all patients).