 A nurse practitioner (NP) plays a pivotal role in modern healthcare, serving as an advanced practice registered nurse with specialized training and expertise. NPs provide comprehensive care, including diagnosing and treating illnesses, prescribing medications, and educating patients on preventive healthcare measures.
A nurse practitioner (NP) plays a pivotal role in modern healthcare, serving as an advanced practice registered nurse with specialized training and expertise. NPs provide comprehensive care, including diagnosing and treating illnesses, prescribing medications, and educating patients on preventive healthcare measures.
With their advanced clinical skills and focus on holistic care, Nurse Practitioners bridge the gap between primary care providers and specialist physicians, offering accessible and high-quality healthcare services to individuals across the lifespan.
If you’re hoping to pursue a career as an NP or a registered nurse (RN) ready to advance your practice, the first step is pursuing relevant education. Duquesne University offers several academic programs, including advanced degrees, certificates and online courses that prepare registered nurses to become nurse practitioners. With multiple areas of emphasis, prospective students can expect to receive a rigorous and fulfilling education that fosters practical preparation for real-time applications to meet their desired career outcomes.
What Is a Nurse Practitioner?
 A nurse practitioner is a registered nurse with an accredited, advanced nursing degree such as a master’s, post-master’s or doctorate with a certification designation. In the United States, there are two main certifying bodies for nurse practitioners: the American Nurses Credentialing Center (ANCC) and the American Association of Nurse Practitioners (AANP). Both organizations offer certification exams for nurse practitioners, and individuals can choose which exam to take based on their preferences and practice focus.
A nurse practitioner is a registered nurse with an accredited, advanced nursing degree such as a master’s, post-master’s or doctorate with a certification designation. In the United States, there are two main certifying bodies for nurse practitioners: the American Nurses Credentialing Center (ANCC) and the American Association of Nurse Practitioners (AANP). Both organizations offer certification exams for nurse practitioners, and individuals can choose which exam to take based on their preferences and practice focus.
Advanced nursing degree programs offer a more intensive look at the duties and responsibilities of nurses, often of the depth and detail required to help them specialize their practice or pursue leadership roles. The overlap in functional care responsibilities between physicians and nurses can be confusing, so it’s important for prospective nurse practitioners to have a solid understanding of their expected roles and responsibilities within their healthcare environment. Here is some information about what nurse practitioners do.
What does a nurse practitioner do?
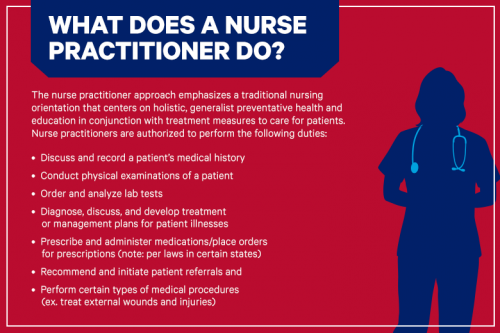
The nurse practitioner approach emphasizes a traditional nursing orientation that can center on holistic, generalist or specialized preventative health and education in conjunction with treatment measures to care for patients. Nurse practitioners are authorized to perform the following duties:
- Discuss and record a patient’s medical history
- Conduct physical examinations of a patient
- Order and analyze lab tests
- Diagnose, discuss and develop treatment or management plans for patient illnesses
- Prescribe and administer medications/place orders for prescriptions
- Recommend and initiate patient referrals
- Perform certain types of medical procedures (ex. treat external wounds and injuries)
Note that the extent of a nurse practitioner’s autonomy depends on the state in which they practice. Some duties and actions may be conducted without supervision or under varying levels of supervision. The AANP link in the sources below provides a comprehensive look at each state’s practice environment.
In the same vein, there are several other actions nurse practitioners cannot perform. Some of those include the following:
- Surgical procedures
- Baby birthing
- Becoming a specialist (ex. ophthalmology or anesthesiology)
- Specializing in specific medical domains (ex. endocrinology, epidemiology, radiology, etc.)
- Practicing independently (note: per laws in certain states)
- Referring Medicaid patients to specialists without a physician’s approval
- Formally advising medical students and fellows
- Referring to themselves as a medical doctor
Consequently, physicians have a broader scope of practice, responsibility and authority in professional medical spaces than nurse practitioners, as they can implement every measure in the list immediately above and more, provided they possess the education, training and certifications to do so.
While nurse practitioners cannot specialize in specific medical domains in the same manner as physicians, they can study to obtain certification in special areas of practice. Examples include focuses such as psychiatry, forensics, gerontology and several others. One of the most popular areas focuses on families, leading aspirants to obtain the ANCC’s Family Nurse Practitioner Certification (FNP-BC) credential. These area-of-practice designators may require specific forms of care pertinent to that area, which can adjust their scopes of practice as-needed.
When considering the nurse practitioner profession, note that in some states, it is mandatory for nurse practitioners to work under the direct supervision of a physician by law. Additionally, nurse practitioners, like physicians, must also ensure that their educational and certification credentials are in good standing with any applicable state laws and state boards, which ensures that they are qualified to act as competent authorities when providing medical care to patients.
Becoming a Nurse Practitioner
Like many other professions, becoming a nurse practitioner is demanding but worthwhile. Every nurse practitioner must possess the necessary educational and certification credentials to obtain employment in a medical facility. While many have taken different paths to become nurse practitioners, one of the most common is as follows:
- Obtain an Associate Degree in Nursing (ADN) or Bachelor of Science in Nursing (BSN).
- Take and pass the National Council Licensure Examination for Registered Nurses (NCLEX-RN).
- Become a nurse practitioner, also known as an advanced practice registered nurse (APRN), by obtaining a master’s or doctoral degree in nursing.
- Select a special area of study during graduate studies to work in a specific setting post-graduation (optional).
- Select an area of study open to NPs/APRNs for certification (ex. adult care, geriatrics, women’s health, etc.) (optional).
There are alternative paths aspirants can take to become nurse practitioners. Some nurse practitioner students choose to complete academic steps before obtaining an ADN or BSN, such as earning certified nursing assistant (CNA) and/or Licensed Practical Nurse (LPN) credentials. Making the decision to pursue either of these credentials can prolong the time necessary to obtain the NP/APRN credential and certification.
Earning the ADN takes most students two years of community college study. Earning the BSN takes four years and typically happens at a traditional four-year institution. The primary differences between the two are the amount of time and money spent to earn them, with the former costing less and the latter costing more. However, BSN programs tend to provide a more in-depth education with the additional two years required to complete them.
Obtaining the master’s degree in nursing alone takes an average of two to four years. However, several institutions offer accelerated programs to save aspirants time and money. Overall, the process of becoming a nurse practitioner is typically completed in a time frame of six to eight years, special circumstances notwithstanding. Aspirants should also account for clinical learning components when calculating time to complete their studies as most programs require several hundred hours of training time in practice and observation.
Understanding the Nursing Structure
The nursing profession encompasses multiple areas of practice, creating several layers of differentiation in the function and placement of medical professionals. However, the core levels of nursing remain the same. Those nursing designations are listed below from the lowest to the highest ranking as dictated by credentialing and scope of practice.
- Certified Nursing Assistant (CNA)
- Licensed Practical Nurse/Licensed Vocational Nurse (LPN/LVN)
- Registered Nurse (RN)
- Nurse Practitioner/Advanced Practical Registered Nurse (NP/APRN)
- Doctor of Nursing Practice and other doctoral designations (DNP)
- Chief Nursing Officers (CNO)
In addition, there are also multiple nursing typologies as determined by focus and areas of practice or certifications. Typologies and specialty areas do not dictate the nursing levels. Instead, they characterize the nature of practitioner’s work at their designated level of nursing.
To that effect, the scope of practice can vary based on specialty areas, but not necessarily in a manner that allows increased authority. In this case, the scope of practice likely contains specific daily tasks or courses of action that may not be common in other areas. Certifications, however, potentially allow increases in the scope of practice and authority as they endow practitioners with advanced or specialized knowledge that other practitioners may not have.
Some of the nurse practitioner typologies include:
- FNP (Family Nurse Practitioner)
- PNP (Pediatric Nurse Practitioner)
- AGNP (Adult-Geriatric Nurse Practitioner)
- CRNA (Certified Nurse Anesthetist)
- WHNP (Women’s Health Nurse Practitioner)
- NNP (Neonatal Nurse Practitioner)
- Cardiac Nurse Practitioner
- Certified Nurse Midwife
The typology or area of practice often determines the type of facility a practitioner works in. Nurse practitioners work in a wide variety of medical facilities or spaces necessitating the services of medical professionals including the following:
- Urgent care offices
- Emergency rooms
- Public health departments
- Private medical practices
- Clinics
- Home care
- Nursing homes
- Hospice and palliative care centers
- Educational facilities
- Specialty medical centers
Becoming a nurse practitioner presents a vast assortment of employment possibilities. With multiple specialty areas, aspirants can choose to work with patients of all backgrounds that require a variety of medical needs. Further, nurse practitioners are uniquely positioned to provide advanced forms of health care to help patients better understand, mitigate and treat illnesses, making this professional pathway ideal for the broad range of medical facilities that regularly require the focus and attention that nurse practitioners offer.